COVID-19 and Public Health in India
The COVID-19 pandemic in India caused considerable suffering, along with economic and social disruption. Till October 2021, 34.3 million people were infected by COVID-19, and an estimated 0.45 million people died. One of the defining features of the pandemic was a public reckoning of the state of the health system. Was the healthcare system in India capable of responding to a large-scale pandemic? What were the economic costs of the lockdowns imposed to control the pandemic? And what is the direction of public healthcare in India?
The Indian Healthcare System
The good news is public health expenditure in India has increased. Revised estimates for 2020-21 place the share of overall spending on health at 1.8% of GDP. The SDG India Index Report (2019-20) by NITI Aayog reports that India aims to increase health expenditure to 2.5% of GDP by 2025. Furthermore, important health schemes such as Ayushman Bharat, launched by the National Health Policy 2017, aim to widen tertiary health coverage.
While these measures are promising, India lags in public health investments and infrastructure, both in contrast to its international peers as well as compared to its own aspirations. Current health expenditure in India is lower than the world average of 9.8% of GDP as of 2018. According to World Bank data, current health expenditure (% of GDP) was 9.51% for Brazil, 5.32% for Russia, 4.12% for Turkey and 2.18% for Indonesia in 2018. India’s federal structure implies that both the centre and state governments spend on healthcare. However, state health expenditure in India is highly divergent, ranging from 3.4% to 12.66% of state budgets, as of 2020-21.
What is more concerning is the health infrastructure investments in India – which fall short of the demands of its large population, and the expenditure levels as well. Total number of government hospital beds per thousand vary widely across states. In 2019, for instance, Karnataka and Kerala had 67 and 61 government hospital beds per thousand, respectively, while states like Punjab and Uttar Pradesh had 22 and 11 government hospital beds per thousand people respectively. Indeed, the covid facility camps and beds may have increased during the pandemic (data not yet available on this), yet disparity in health infrastructure across states is a standing issue.
Economic Costs of the First Lockdown
During the first wave of infections in India in March-May 2020, the Government of India implemented the “world’s strictest lockdown” (Hale et al. 2020). This lockdown severely disrupted business activity and mobility, with millions of migrants traveling back to their villages as opportunities for work in the cities dried up.
The rationale behind implementing this lockdown was to curtail the spread of Covid-19 and to reduce the consequent burden on the healthcare system to save lives. The government hoped that the lockdown would allow for a quicker resumption of normal economic activity over time. However, the trade-off from the lockdowns was short-run reductions in economic activity. In contrast to wealthier countries, the lockdown potentially affected the Indian economy more as per capita incomes were lower; remote working was less prevalent; the extent of digitisation was lower, and social protection was weaker.
What was the economic cost of this lockdown? One perspective is that Gross Domestic Product (GDP) contracted by 24.4% in the second quarter of 2020. However, this headline number conflates both lockdown effects, as well as potentially self-imposed restrictions as citizens restrict their own activities due to the spread of Covid-19 infections. To isolate the impact of government-imposed restrictions (separately from other factors), Beyer, Jain and Sinha 2020 examined the economic implications of a graded ‘unlock’ in May and June 2020, when the central government decided to vary containment rules across districts in the country).
The Impact of Zonal Containment on Economic Activity
The Government of India announced a comprehensive nationwide lockdown on 25 March 2020, which was implemented uniformly across all states and districts. During this phase, nearly all offices, commercial and private establishments, industrial units, as well as public services were closed. Most transportation services – including international and domestic flights, railways, and roadways – were suspended. Hospitality services and educational institutions were shut. This nationwide lockdown lasted until 3 May 2020.
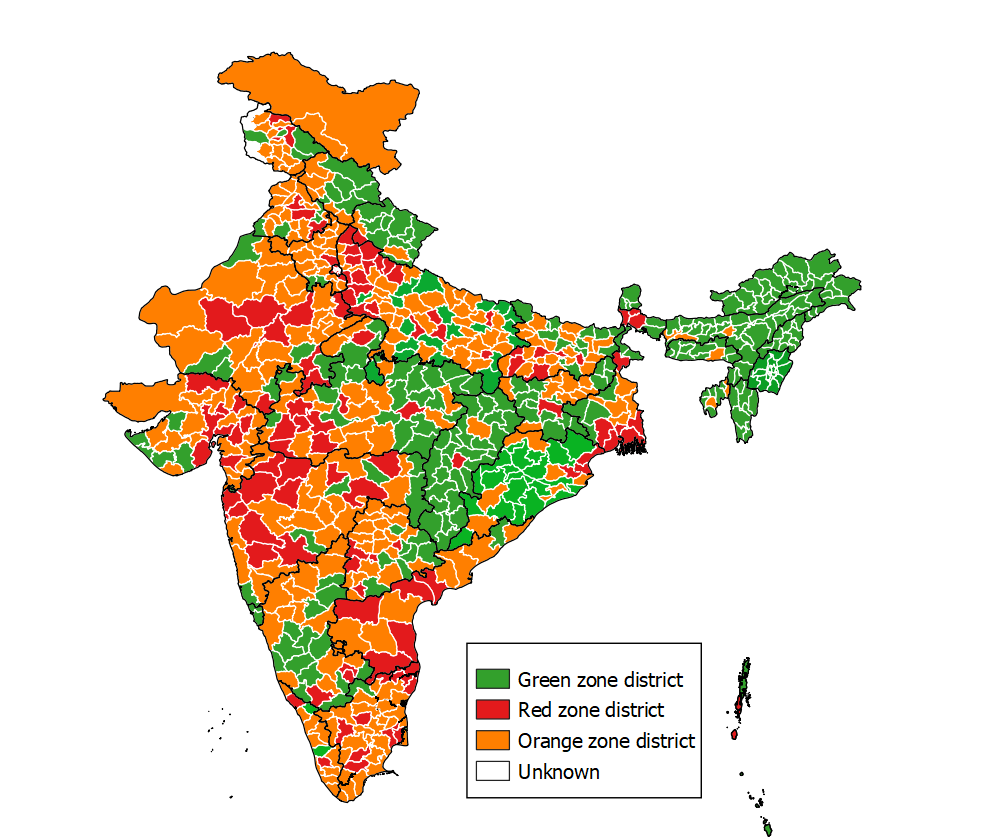
To facilitate a gradual resumption of economic activity, the government announced in May 2020 a differentiated unlock of districts, with some districts retaining strict restrictions, some with intermediate measures, and the remaining districts returning to “business as usual”. The authors of this article contrasted how these districts fared on a range of outcomes – individual mobility (measured by location tracking on cell phones), economic activity (measured by satellites from outer space), and household consumption and income (measured by household surveys).
What were the findings? First, phone location data corroborated that the restrictions were indeed effective in reducing mobility, as the government mandated. The main finding is that the economic recovery was lower by 9.3% in districts with the maximum restrictions relative to districts with minimal restrictions. The recovery was 1.6% lower in districts with intermediate restrictions compared to districts with minimal restrictions. These results are not driven by India’s large metropolitan cities and hold even when they are excluded from the analysis. Some districts were more impacted by the restrictions than others. More developed districts with above-median population density, share of employment in services, credit per capita, and average age, experienced larger impacts.
Households reported both lower income as well as reduced consumption as a consequence of the lockdowns, worrying for the long run if this impacts human capital investments in nutrition, health, and education.
India suffered a lot less economically during the second wave of the pandemic due to imposition of micro-containment zones, in contrast to nationwide lockdown during the first wave. Policymakers can continue to follow similar approaches and maintain preventive measures and protocols which could enable least disruption to economic activity, trade, and travel even as threats of further variants emerge.
Policy Trade-offs
Could greater public health expenditures insure against the need for large scale lockdowns in future health emergencies? For policymakers, GDP decline estimates offer a useful benchmark to contrast with public health expenditures.
India’s economic policymakers well understand the value of increased investments in healthcare. During the pandemic, Indian public health expenditure rose from 1.5% of GDP to 1.8% of GDP. The PM Ayushman Bharat Health Infrastructure Mission scheme aims to increase infrastructure, with financing from the central government. Furthermore, the private sector played a major role during the pandemic, from the development and manufacture of vaccines, to diagnosis of COVID-19 infections and vaccination. To prevent high prices, the government regulated private sector with extensive price controls. Whether this expansion of private sector activities sustains (both in COVID-19 related and other healthcare needs) is an open question.
The way forward should involve building public consensus on the importance of healthcare investments and recognizing the potential economic gains from greater investments.
Disclaimer: The views expressed in the article are those of Dr. Sinha and Prof. Jain and not the Reserve Bank of India. The usual disclaimer applies.

Dr. Sonalika Sinha, Economist, Reserve Bank of India |

Prof. Tarun Jain, Associate Professor of Economics, Indian Institute of Management Ahmedabad |
Further Reading:
Beyer, R., T. Jain and. S Sinha (2020), ‘Lights out? COVID-19 containment policies and economic activity’, World Bank Policy Research Working Paper 9485.
